-

BECAUSE EVERYONE
DESERVES TO HAVE ACCESS TO GREAT KIDNEY CARE702.877.1887 HOURS: MON-THUR 8AM – 5PM, FRI 8AM – 12PM -

BECAUSE EVERYONE
DESERVES TO HAVE ACCESS TO GREAT KIDNEY CARE702.877.1887 HOURS: MON-THUR 8AM – 5PM, FRI 8AM – 12PM
Patient Resources
Kidney Specialists of Southern Nevada provides comprehensive kidney care and a full spectrum of kidney disease management resources for residents of Southern Nevada. Our nephrologists educate and empower patients who are living with kidney pain, infections, stones, and other kidney problems. We are a patient-focused practice committed to slowing the progression of kidney disease and maximizing your quality of life.
What we do
KSOSN offers the region’s most comprehensive kidney care services. We have assembled an entire team of caregivers–physicians, nurse practitioners, nurses, medical assistants, and patient care coordinators–to both treat and educate patients on how best to manage their kidney disease. Our nephrologists and caring staff will help you manage your kidney disease with knowledge and leading edge medical treatments. Our goal is to improve your quality of life by providing you with the tools to prevent, or delay as long as possible, the need for dialysis.
You are the most important person on the KSOSN team.






Care Team
Services
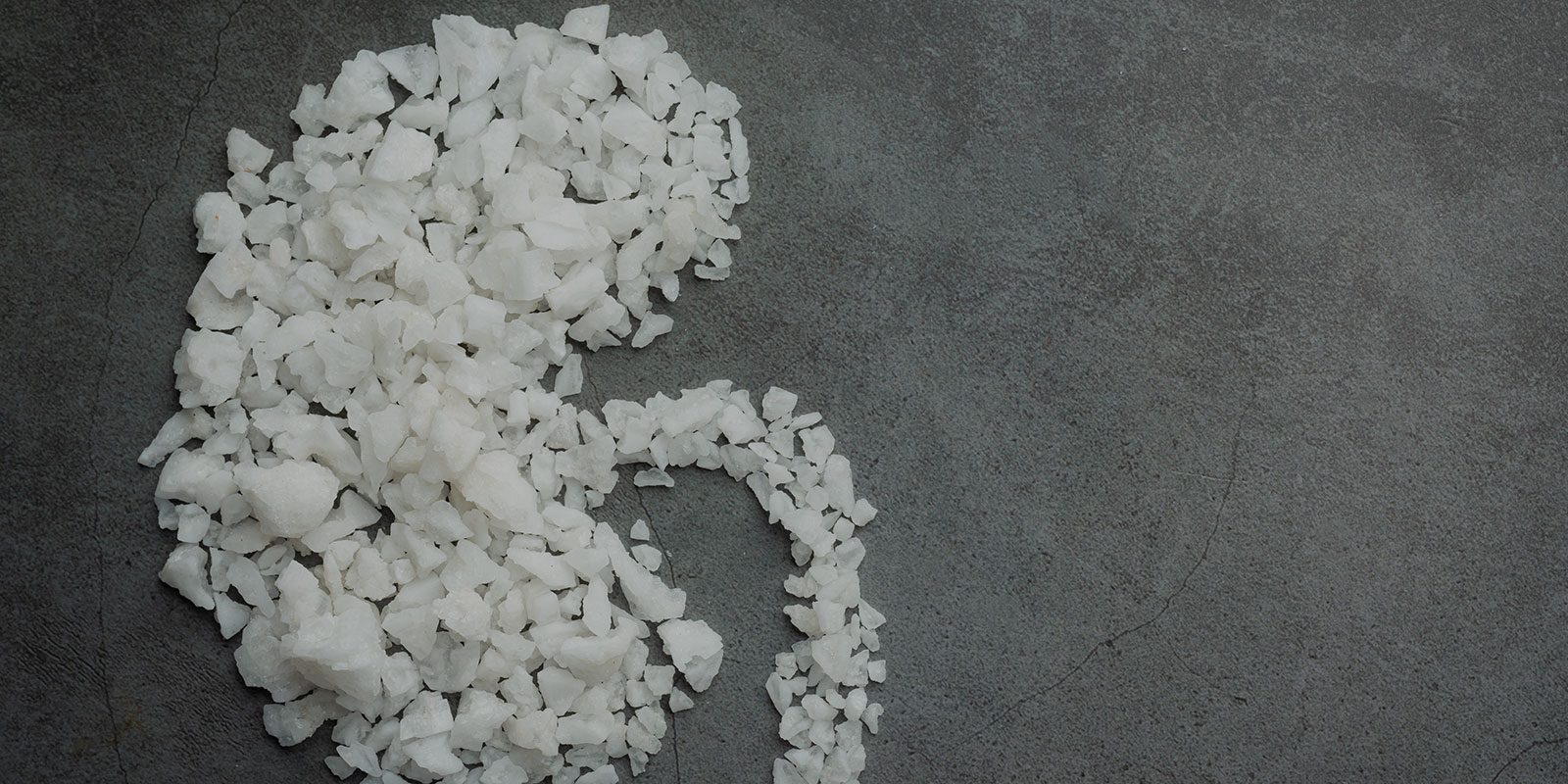
Chronic Kidney Disease
READ MORE
Kidney Transplant
READ MORE
Home Dialysis
READ MORE
Hemodialysis
READ MORE
Research
READ MORE
Polycystic Kidney Disease (PKD)
READ MORE
Complete Dialysis Access Care
READ MORE
Kidney Disease Education
READ MORE
Remote Patient Monitoring
READ MORE
Anemia Management
READ MORE
High Risk Patient Care
READ MORE
Second Opinions
READ MORE
Kidney Specialists Surgical Center
READ MORETestimonials

My Doctor Kevin Yu, MD. and his medical assistant, Vanessa, are a wonderful team, efficient and dedicated to the patients. I, as a patient feel great knowing that I can leave a voicemail and my call is returned promptly. It gives me a great deal of comfort and I am given the up most care and understanding. Vanessa takes time out of her day to listen to my issues and get them resolved. She is really a beautiful diamond!
If all medical offices were like the staff at KSOSN, it would be a much better and efficient world! I am proud to have them on my team taking care of me and they never disappoint me. I am so blessed. All the staff at KSOSN are awesome and remarkable and work as a great team to help everyone. Each patient is treated like Royalty and special. It feels really great to see my specialist and his assistant. I appreciate and thank them!
Geraldine
Jan, 2023
Thank you Dr. Boldur and entire clinical team for supporting my uncle throughout Chronic Kidney Disease progression, End Stage Renal Disease and now TRANSPLANT! The true gift of life was shared, and our family truly appreciates Dr. Boldur, and all teams involved to make his transplant possible.
Kasandra
Feb, 2024
All staff are friendly & professional. Dr. Yu reviews my lab results, explaining how I can improve by changing some behaviors. He is encouraging & understanding.
Ruth
Dec, 2022
Dr Corbin is great. She listens to you and cares about your concerns. She explains why she is recommending a test so you understand the process.
Joann
Dec, 2022
Dr. Yang thoroughly knows my current and past history .He is very approachable, pleasant, intelligent, knowledgeable & I totally trust him. I I recommend him highly.
Felimar
Dec, 2022
I have been with KSOSN since Dec 2013. I am very grateful for their expertise in dialyzing me. The staff and technicians are professionals and caring. They are prompt to respond when we need assistance. I am very satisfied with their services.
Isabella
Jun, 2022
I have been a patient of Dr. Syed Shah since I had my kidney transplant in July of 2014. I have been so blessed and grateful to find such an amazing doctor. Dr. Shah is very knowledgeable, kind and will help you. He will take care of you and listen to your concerns. As a kidney transplant patient, it is very important to me that my relationship with my doctor is great and will help guide me with important decisions in my health. I couldn’t be happier with Dr. Shah and his staff.
Maharlika
Jun, 2022
Dr. Kevin Yu treated my father at Valley Hospital last month. Miracles do happen! My dad received a transplant. He never would have made it to that moment if Dr. Yu did not fight for him and for our family by being creative and not willing to give up on us. It was looking really bleak when we left Valley. I don’t think anybody expected dad to survive …but he did! And he is doing great. Dr. Yu made a difference. We are so grateful that everything actually worked out.